The parotid is the largest of the salivary glands. It lies wedge-shaped between the mandible and the sternocleidomastoid.
Superiorly, it is related to the external auditory meatus and the temporomandibular joint, whereas inferiorly, it is attached to the digastric. Anteriorly lies the masseter muscle. Medially, the styloid process and its muscles separate the gland from the important vessels such as the internal jugular and the internal carotid artery and the last of the four cranial nerves IX, X, XI and XII.
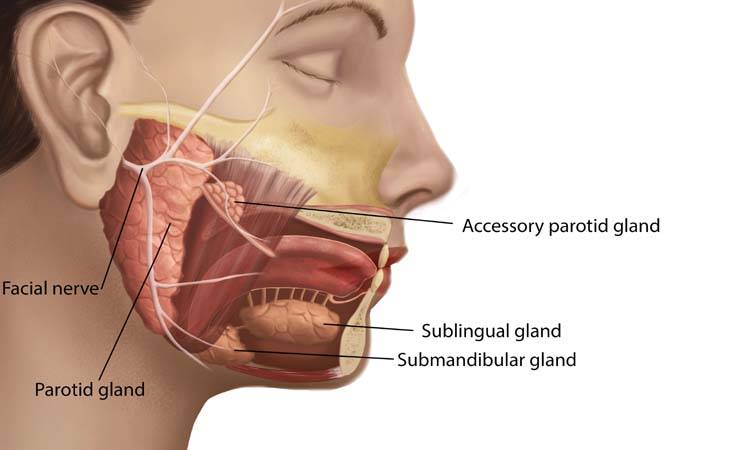
The gland is divided into superficial and deep lobes by three structures traversing the gland, The facial nerve, the Retromandibular vein (superficial temporal+maxillary vein) and the External carotid artery near the neck of the mandible.
The parotid tumours are the most frequent salivary gland tumours. Malignant parotid tumours are rarer than benign but can appear very similar to a benign process as they grow at a slower pace and displace rather than infiltrate the neighbouring structures compared to other malignant tumours of the head and neck. It is, therefore, crucial to adopt a stepwise management approach for parotid masses that makes early detection and definitive treatment of parotid malignancy possible. Around 80% of the parotid lumps are benign. The most common benign neoplasm of the parotid is a Pleomorphic Adenoma followed by Warthins’ tumour other epithelial masses like oncocytomas, myoepitheliomas, lymphadenomas, lymphomas and other soft tissue tumours like hemangiomas and lipomas[iii].
The most common malignant tumour is the Mucoepidermoid Carcinoma, followed by Adenoid Cystic carcinoma. Even the best imaging and optimal FNAC can never completely rule out a parotid malignancy.
After a thorough history and good clinical examination reflecting the onset of disease, associated symptoms like dysphagia or facial nerve weakness, neglected masses for longer periods, palpable neck nodes and relative resistance to mobility than benign masses, and ultrasonography should immediately be done as ninety per cent of parotid tumours originate in the superficial lobe. High-resolution ultrasonography will precisely demarcate the tumour borders, detects multiple or bilateral lesions, excludes non-neoplastic causes like sialadenitis and sialolithiasis with the added benefit of low cost and zero radiations when a large tumour extends into the parapharyngeal space and attains a “dumbbell” shape. The waist like constriction appears at the region of the stylomandibular ligament. Such tumours may have accompanying symptoms of hoarseness of voice or even sometimes features of Horners’ syndrome.
MRI is the method of choice if a malignancy is suspected after the US-guided Fine needle aspiration Cytology. In cases where no histopathological investigations have been carried out, an MRI provides information on the exact localisation and extent of the lesion, detects perineural spread (ACC), bone invasion and deep infiltration into the parapharyngeal space. A better investigation of choice is a core biopsy with an 18 gauge needle in cases where Fnac shows inconclusive results. Though beneficial, any core needle biopsy risks tumour seeding along the needle’s path and is much more painful than an FNAC. It obtains a tissue that allows both histopathological diagnoses as well as immunohistology. The use of an open biopsy is generally controversial because of the risk of tumour spillage. An excisional biopsy can also cause CNVII paralysis and fistula formation.
When deciding upon the extent of surgery for benign parotid tumours, the main factors to consider are tumour site and size and the histological phenotype(low grade, high grade with extracapsular extension). The most authentic approach for a lump in the superficial lobe is partial or superficial parotidectomy. For deep lobe tumours, the resection of choice would be a total (benign)or radical(malignant or with perineural involvement)parotidectomy with or without a neck dissection.
It is to note that temporary facial nerve dysfunction after parotidectomy occurs in 20-40% of cases, but permanent paralysis is rare0-4%. Routine use of EMG facial nerve monitoring has lowered this incidence.
The surgical anatomy is critical to understand for both facial and reconstructive surgeons. The main trunk is commonly identified as the tragal pointer (1cm deep and 1cm inferiomedial) and the medial attachment of the posterior belly of the digastric(1cm deep). For tumours located in the superficial lobe,i-e superficial to the terminal, branches of the facial nerve, the first step is to identify and locate the main trunk of CNVII originating from stylomastoid foramen entering into the gland. Confirmation can be made with the help of a nerve stimulator.
Following important measurements are of surgical value when resecting a parotid lump:
- The distance of the temporal branch from the root of the zygomatic arch(0.8-3.2cm)
- Superioinferior and mediolateral distance of maxillary artery from the condylar tip (21-24mm&4-8mm)
-The mean distance of the maxillary artery-sigmoid notch junction to the tragal pointer was 22.9 mm (range, 20.95 to 25.05 mm).
Paraguay Line, a line drawn 0.5 cm inferior to tragus to 1.5cm superior to lateral eyebrow, represents the temporal branch of the facial nerve.
The zygomatic branch is identified at a mean OF 30.71mm anterior to tragus at the anterior border of the gland and 19.2mm inferior from the midpoint of the tragus and the lateral palpebral commissure.
Zukers’ Point-represents the buccal branch and is a midway point on a line drawn from the root of the helix and the lateral commissure of the mouth.
The marginal mandibular branch has variable anatomy but is usually encountered within 2cm below the body of the mandible. The cervical branch can be found 1cm below a perpendicular line drawn from the angle of the mandible to a line from mentum to the mastoid process. Its injury has little functional consequence.
In cases of Recurrent (or residual) pleomorphic adenomas, causes of recurrence may include capsular rupture, satellite lesions, pseudopods and grossly positive margins. Biologic and genetic factors may also play a role, which is out of the scope of this review. Such tumours possess a high risk of facial nerve complications as anterograde identification becomes difficult in redo operations. Literature supports a retrograde identification of facial nerves in such cases. In few cases, removal of the mastoid tip has also been done.
For tumours located in the deep lobe, surgical approaches of choice include an Atransparotid approach with mandibulotomy, a Transcervical approach or a combined trans parotid-transcervical approach. Trans parotid is preferred for tumours going from the superficial to the deep lobe.
Malignancy can arise in three forms from a Pleomorphic adenoma
a-carcinoma ex pleomorphic
b-carcinosarcoma
c-metastasising pleomorphic adenoma
Prognosis is difficult to quantify for malignant pleomorphic adenomas because it is not widely reported.
Treatment of Recurrent benign tumours proving better disease control is a wide local resection followed by radiotherapy. For malignant cases, NCCN guidelines suggest an elective neck dissection along with primary tumour resection.
The most frequently involved neck levels in Parotid cancers are II, III, IV. Level I and V can also be involved in high-grade tumours. It means that a therapeutic neck dissection must include all levels from I to V.In clinically No necks, some surgeons prefer supraomohyoid neck dissection. In contrast, some also consider removing level IV as well.
Surgeons have to pay attention to minimise the risk of complications during parotidectomy. Good surgical techniques with multiple anatomic landmarks, preop discussion and consent, what to expect post-op and description of major and minor complications associated with the surgery are vital in reducing complications and acquiring patients’ trust and confidence. Patients also need to be informed about the cosmetic sequelae, the possible hollowing defect and its reconstruction pre or post-op; CNVII paralysis or paresis is possible, can be partial or total, temporary or permanent.

Dr Saqba Alam
The author is a contributing writer at Dental News Pakistan and a fellow of Maxillofacial Surgery. She can be reached at drsaqbaalam@gmail.com

